FAQs
General FAQs
How do I make an Appointment?
Simply call us at (770) 363-8770(770) 363-8770 during our working hours or you can request an appointment online using this form.
Do I need a referral to make an appointment?
Most medical specialists will accept only referred patients. This is mainly to try to ensure that the specialist you are seeing is appropriate for you and your condition. Check with your insurance company to see if a referral is necessary.
What to bring for your initial consultation?
For your initial consultation you will need to bring a referral letter from your physician if necessary.
Here is a check list for your initial consultation
- Driver’s License or a valid ID
- Insurance information
- Referral Letter (if required)
- Reports, X-rays, MRIs, CT scans etc. and any other relevant information
- List of medications (if any)
We encourage you to come to your initial consultation with a written list of questions to ensure you don’t forget to ask them when you are seeing the doctor.
Are my medical records kept private and confidential?
Your medical file is handled with the utmost respect for your privacy. Our staff is bound by strict confidentiality requirements as a condition of employment regarding your medical records. We will not release the contents of your medical file without your consent.
How long do I need time off work after the surgery?
The post-operative recovery period varies based on the particular surgery. Generally, it is recommended patients take two weeks off work to recover from any surgery and to resume light duty following resumption of work. Your surgeon will give you specific instructions to follow for a successful recovery.
How long before I can resume driving?
You should wait at least one week before driving after surgery. The effects of the anesthetic and surgery can affect judgment and reflexes during the first week following your surgery. Your surgeon will provide more specifics for your particular situation.
When can I resume exercise?
Your doctor will instruct you about post-treatment exercises – the type and the duration to be followed. You may be referred to a physical therapist to help with strengthening and range of motion exercises following surgery.
How do I contact the doctor or staff after hours?
There will be a point of contact 24 hours a day for any concerns you may have. You will be provided with contact details following your treatment.
Medical
What are the non-surgical treatment options?
The non-surgical treatment options include rest, medications including analgesics and antibiotics, injections, and physical/occupational therapy.
Will physical therapy be required after surgery?
Getting full range of motion, strength, and flexibility back after surgery usually takes time. That is where pre-operative exercise, education, and post-operative physical therapy programs come into use to ensure you are physically and emotionally prepared for surgery and to maximize your recovery after surgery.
What are the risks associated with surgery?
As with any surgery, risks include reactions to anesthesia, bleeding, infection, stiffness and nerve damage. Your doctor will discuss the risks associated with your specific procedure.
When can I return to daily activities?
This varies depending on the type of procedure undergone, and can range from a few days to a few months. Return to all activities, sports and exercise can take up to four to six months. Your doctor will advise you depending on your particular health condition.
What can happen if surgery is avoided?
Some complications of not undergoing an orthopaedic surgery for your condition include pain, loss of joint motion, joint weakness, numbness and an early onset of arthritis.
What are the most common injuries?
The most common orthopaedic injuries are sprains and strains, fractures, and dislocations. Injuries can occur when playing indoor or outdoor sports or while exercising. Sports injuries can result from accidents, inadequate training, improper use of protective devices, or insufficient stretching or warm-up exercises.
Surgery Before, During, and After
Before your surgery:
Several steps go into the pre-surgical process.
First and foremost, Dr. Hyman will determine with you if there are any reasonable NON-SURGICAL options to help your condition. He prefers to see you get well without surgery if at all possible. Don't worry, you won't find him overly aggressive to operate on you! Unfortunately, by the time most patients get to us, they have already had prolonged months/years of pain, failed physical therapy, exercise and activity modification, and medications. While physical therapy, acupuncture, chiropractic, etc can be of value in select instances for the soft tissues around the hip, most problems related to the actual hip joint do not get better with these techniques.
Once you and Dr. Hyman agree that hip arthroscopy is right for you, the preparation process includes the following: even more patient education, insurance authorization, and surgery scheduling. Dr. Hyman will further study your case and imaging studies and make sure no further data is needed. A week or so prior to your surgery, you will come in for a 'pre-operative visit' wherein you will have all questions answered and a re-exam and a risk/safety assessment to make sure you get the best care possible. Your 'informed consent' forms will be completed. Special needs equipment is confirmed. (We do adjust our pre-operative visit schedule to accommodate International or out of state patients who may need to come a day or two early and stay at a local hotel)
During your surgery:
You arrive at the facility about 1.5 hrs prior to your scheduled surgical time. After checking in at the registration desk, you will go to the PRE-OP area where you will take off your loose fitting clothes (sweats are good) and get into a hospital gown. All your belongings are safely organized. You will have a review of how to use your crutches for after surgery. They will confirm that you have not had anything to eat or drink since midnight and your hip is cleaned and scrubbed in preparation for the surgery.
You are transported via bed to the PRE-OP holding area just outside of the Operating Room. There you will meet up with your O.R. nurses, the anesthesiologists, Dr. Hyman and his Physician Assistant, Danelle. Your last minute questions are answered. This is your last chance to use the restroom too! Then you say goodbye to loved ones and you are wheeled into the O.R. Setting you up in the O.R. requires you to be transferred to an O.R. bed and putting a warming blanket on you. The anesthesiologists will then put you to sleep and Dr. Hyman and Danelle will pad you and position you comfortably on the traction table. Your legs are put in little foot boots and a fluffy pad is placed in the groin area.
The outpatient hip arthroscopic surgery typically lasts 1-2 hours, depending upon the complexity of your condition. Afterwards, you are transferred to the recovery room and Dr. Hyman will discuss your case with friends or family who are taking you home. In the recovery room, you will have an ice pack on your hip and lots of TLC and some medication. Your feet will be wrapped up with a pillow to prevent your legs from rolling around and irritating your hip. You will also find yourself wearing medical stockings (TED hose) to help prevent the already unlikely issue of Deep Venous Thrombosis (DVT or blood clot). The nurses in the recovery room will monitor your condition and once they and the anesthesiologist feel it is safe for you to go home, they will go over the discharge plan with you and whoever is taking you home. You are wheeled out to your car and off you go.
If you'd like more details of the surgical process, see the Surgical Technique page.

After your surgery:
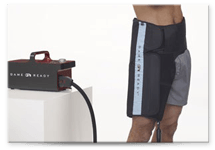
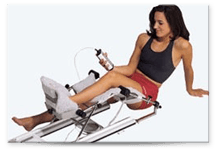
The first few days at home are challenging. If possible, it's best not to have to go up / down a lot of stairs in the first two weeks. It's doable but not ideal. Getting in / out of cars is also challenging. Between surgery and your first post-operative visit, you will will be at home and using an ICE PACK or CRYOTHERAPY device several times a day and may also be using a CPM for 4-6 hours a day, set to 0-60 degrees. This will help the range of motion of your hip joint. We ask that you not bend your hip past 90 degrees so you don't irritate the joint and cause excessive inflammation.
Most patients are using crutches with both legs extended (ie the operated leg hangs straight down but you just don't put weight on it for 2 weeks, possibly four. Dr. Hyman and/or his PA, Danelle Toole, PA-C will let you know. You will wear the white TED hose stockings until your first follow-up visit with Dr. Hyman. At this first visit, you should plan extra time and will have a session of PT with Katheryn, our exceptionally experienced and excellent physical therapist. Even if you are ultimately doing your physical therapy elsewhere, they can give you good advice.
You will have a pillow between your feet while lying in bed, so your legs do not roll inwards or outwards for excessive periods of time. Most patients tolerate this but if you cannot sleep with the pillow, and you can lay still, it is okay to go without it.
When you come into the office for your first post op visit, someone will need to drive you. At that visit, we will review your case, give you the pictures of the inside of your hip and return your radiology studies to you. We will outline your rehab program and make sure all is well.
Who will be taking care of you and your surgery, other than your surgeon?
Once the patient and the surgeon agree that surgery is the best treatment option, a lot of things go into the patient's surgical experience, and ultimately the OUTCOME. You probably are not aware of how many people are involved in ensuring a good surgical result for you, but if you're interested to know, read on.
In our society, the surgeon is presumed to take ultimate responsibility for the patient's care and surgical results. However, in reality, there are a great many individuals, not directly under the surgeon's control, that will also affect the patient's surgical result. Some of them you'll meet along your 'surgical journey,' many of them you'll never know existed. It is important, however, to realize that any one of these people can have an impact, good or bad, on your surgical experience and final outcome.
These people have varying levels of education, expertise, attention to detail, motivation, and standards of excellence. The point is, choose your doctor well, but also hope that the supporting staff that works with you are upholding the same level of care provided by your doctor. In short, it's not just the doctor you need to worry about.
The following list is in chronological order, starting from the first people involved in your surgical journey, to the last people involved when your care is completed. If any one of these individuals is not giving their full, undivided attention to your care, (and sometimes even if they are) you could experience a complication/bad outcome. Your surgeon will likely be assigned the blame, but read on to see who all are really involved. Your surgeon doesn't supervise or interact with most of these people. As you'll see, other than your surgeon, there are more than thirty (30) people who impact you.
Before your surgery:
- Pre-operative nurse- This person will do your initial screening before surgery and assess your health risks for anesthesia. If they detect some risk factor, they may send you to your PCP for further screening. Click Here to download the Bleeding & Clotting Risk Factors PDF form.
- Your primary care physician (PCP) - Depending on your age, your PCP may be asked to provide a note stating that you are in as good a medical condition as you reasonably could be - in anticipation of your upcoming surgery. Often they will order some blood work.
- The phlebotomist - This person draws your blood. Poor technique can contaminate your blood sample or cause infection from the needle.
- The laboratory technician - If you have any blood work or labs ordered by your doctor, the lab tech must process the blood properly and give accurate results.
- The nursing secretary - This person takes the doctor’s written medical orders in your chart and enters them into the computer, including medication types and dosages.
- The radiologist - This doctor reviews your X-rays, ultrasound and MRI, and determines the official result.
- The radiology/MRI technician - This person is the individual who actually does your MRI, and sets all the parameters for your study. The doctor is NOT usually present during this test.
- The EKG technician - This tech sets up this test to determine if your heart is beating properly.
- The surgeon's staff/medical assistants/nurses - They will complete your paperwork with you, and give you your prescriptions and instructions.
The day of your surgery:
- The pre-surgery holding area nurse - After you check in, this nurse will get you 'prepped' which will include putting in an IV catheter in your arm, and possibly shaving the area of the surgery. Poor technique can lead to infection.
- The nurse anesthetist - This person will get you ready for anesthesia and be administering most of your anesthetic medications. Needles will be used and medication vials will be opened. They will also determine how much 'gas' you get. They will be with you throughout the surgery, but they often rotate to give each other breaks. Therefore, you may have 2 or 3 nurse anesthetists attending to you while you are asleep. They are also responsible for checking to make sure your body is in a padded and protected position throughout the surgery. Poor technique can lead to death or permanent functional damage.
- The anesthesiologist – If required, this doctor will be present to supervise your nurse anesthetist by occasionally coming in the operating room to 'see how things are going.' They are often present at the beginning and end of your surgery. The anesthesiologist also confirms that the position of your body (sitting up, laying on your side, your back, or your stomach) should be safe for your surgery. Poor technique can lead to permanent functional damage.
- The scrub nurse - This person will be handing the instruments to the surgeon, and assembling all the gadgets that the surgeon uses. These individuals often rotate, and in a hospital setting, may have no experience with orthopaedics or with the surgeon's techniques. Improper techniques can lead to infection, broken implants, delaying the surgeon and incorrect devices implanted.
- The circulating nurse - This person walks around in the operating room, recording the medications given, the time things happen, and hooking up different types of equipment for the surgeon's tools. They may have to open sterile equipment and also prepare sterile materials/solutions that will ultimately go into your body. Improper techniques can lead to infection, delaying the surgeon and incorrect devices implanted.
- The surgical assistant tech (SA) - This person assists the surgeon by holding equipment or tools when the surgeon's hands are full. They sometimes sew wounds closed or may even be asked by the surgeon to operate some of the tools.
- The physician assistant - This person assists the surgeon by holding equipment or tools when the surgeon's hands are full. They sometimes sew wounds closed or may even be asked by the surgeon to operate some of the tools.
- The implant/devices equipment rep - This individual brings in (from their office or the trunk of their car) special devices that will be used on you or implanted in you. They will also instruct the scrub nurse on how to properly assemble these things for the surgeon's use.
- The orderly help in the operating room - These individuals help transfer you on and off the operating room table while you are 'out of it.' Forceful movements could damage the surgeon's work, or injure you.
- The sterilization staff - These individuals stay in the 'laundry room' of the OR. It is their job to clean, wash, rinse, scrub, and sterilize all the surgical tools. Poor technique can lead to infection or broken tools.
- The housekeeping staff - These individuals clean the room (operating room or hospital room) in between patients to decontaminate and remove harmful germs. Poor technique can lead to contamination of your surgery.
- The recovery room nurse - This nurse will monitor you while you wake up in the recovery room, giving you pain medication, and checking you for signs of complications from your surgery. He/she will also adjust your sling, brace, splint or cast, and apply an ice pack to reduce swelling. The setup of these devices can affect your results. Lack of attention here can lead to death or functional impairment.
- Recovery room x-ray tech - Often, before you wake up in the recovery room, an X-ray will be taken of your operated area. This person will move you around to position you for the X-rays.
- The floor nurse - If you stay in the hospital overnight, a nurse will watch after you, usually a different nurse every 8-12 hours. The night nurses are more likely to be foreign graduates.
- Your pharmacist - This person is responsible for filling your prescriptions the way the doctor ordered, and checking to see if there might be any bad drug reactions from the medications. Filling this inaccurately can lead to nausea, pain or worse.
After your surgery:
- Your family or friends - Depending upon your resources, you may have other people assisting you, giving you advice and impacting your recovery. Unless you live with your surgeon, that assistance or advice may not always be 100% correct.
- Visiting nurse - If you have a nurse come over to your house after surgery. He/she will be assisting you, giving you advice and impacting your recovery.
- Hospital staff - If you are admitted to the hospital, you'll be meeting some of the above people again; having your blood drawn, orders transcribed, more tests, more interpretations and more nursing care.
- The physical therapist - Soon after your surgery or discharge, you will likely begin some form of the physical therapy / rehabilitation. This person will help you move your injured body part around to aid in recovery. Therapy that is too aggressive can cause pain, re-injury or inflammation. Therapy that is not aggressive enough can lead to weakness, stiffness and a loss of function.
- The surgeon's medical/clinical staff/nurse/PA - These people work for the doctor, and they will be returning your phone calls, acting as an intermediary between you and the surgeon, giving you medical advice, calling in prescription re-fills, renewing therapy orders, and filling out forms. Lack of attention to detail here could impact your recovery.
- Durable medical equipment rep - This person may fit you with a brace, sling, boot, cast or mechanical medical device to aid in your recovery. The setup of these devices can affect your results.
- Home equipment rep - This person may come over to your house to set up or deliver home equipment to aid in your recovery. This individual transports these items from their office or the trunk of their car. The setup of these devices can affect your results.
- Special equipment rep - This person may be called on to set you up with a special medical device, eg bone stimulator or oxygen tank, etc. The setup of these devices can affect your results.
- The workers at your insurance company - This institution controls payments for all the above services. If they refuse to pay for your care or grant you the benefits of these services above, it could delay or inhibit your timely recovery.
Ultimately, you, the patient, can have the biggest impact on your care. IF all these people above (and your surgeon) do their best, and IF you have good fortune, you still have a lot of work to do for your best shot at a great result. You should:
- Follow the post-surgical guidelines
- Communicate your concerns if some arise
- Avoid harmful products like tobacco, alcohol and recreational drugs
- Take your medications as prescribed
- Complete your physical therapy as prescribed
- Do your home exercises
- Be patient with yourself
- Be optimistic, but realistic
- Expect some ups and downs along the way
- Make sure you understand 'the plan' for your recovery
Driving After Surgery
Typically, one would have difficulty driving for about 2-3 weeks, though you might be able to drive short distances within a week after surgery. It all depends on pain, swelling, stiffness, type of car, side of surgery: right vs. left, etc. Most patients do NOT drive AT LEAST until after their first postoperative visit (7-10 days after surgery). Even then, caution should be exercised, especially if you are on pain medication or if mobility is limited.
- Reflexes and coordination are often somewhat impaired for several weeks after surgery, so care should be taken to drive slowly, with extra distance between cars, etc.
- Most people are able to resume relatively 'normal' driving about six weeks after surgery.
- You must regain adequate muscle control for braking and accelerating before you try to drive.
- Contact your auto insurance company to see if they have any additional restrictions/exclusion clauses on driving after surgery.
Please read this BBC News article: Patients Warned Over Driving After Surgery
Flying After Surgery
For surgery on the arms and upper extremities, the risk of developing blood clots, etc., AFTER surgery is unknown, or thought to be very low. No one knows the true risk. In my experience, one week is fine. I've never had anyone get a blood clot with those guidelines.
Deep vein thrombosis occurs when flying long distance because you are sitting down for long periods of time with limited opportunities to move around. You are also more likely to become dehydrated. Dehydration can cause the blood to become thicker than usual. Deep vein thrombosis is often referred to as Economy Class Syndrome. This is incorrect as people sitting in first class are equally at risk. Deep vein thrombosis can happen in other types of long journeys as well.
When flying you should follow these guidelines set by British Airways:
- Drink plenty of non-alcoholic fluids.
- Avoid drinking alcohol and drinks with caffeine, such as tea and coffee.
- Avoid smoking.
- Stand up in your seat area and stretch your arms and legs.
- Get up and move around as often as you can (at least twice an hour).
- When sitting, try moving your ankles around and going up and down on your tiptoes.
- Avoid sitting with your legs crossed.
- Avoid wearing tight clothes, especially socks or tights that are too restrictive.
- Seek medical advice before travelling, if you have a previous history of deep vein thrombosis or you believe you might be at risk.
Further information from PreventDisease.com: Flying Far? Watch for DVT
Surgery and Smoking
Smoking and the musculoskeletal system:
Smoking can take a significant toll on the musculoskeletal system. Tobacco and nicotine increase the risk of bone fractures and interfere with the healing process, according to a growing body of research. Nicotine can slow fracture healing, estrogen effectiveness, and can counter the antioxidant properties of vitamins C and E. At a 2002 meeting of the American Academy of Orthopaedic Surgeons, research on the topic of smoking and its effect on the musculoskeletal system was reviewed. Some of the orthopedic problems caused by smoking include:
- more severe disc degeneration
- weakened spinal ligaments
- reduced production of bone cells
- faster bone loss in postmenopausal women
- fractures take longer to heal
- rotator cuff surgery is less successful
- longer healing time for surgical incisions
- more post-surgery complications
- delayed spinal fusion
However, quitting smoking seems to improve the healing process in most cases, except for long-term, heavy smokers who have permanent artery damage, according to the researchers. Those with permanent artery damage due to smoking may not heal easily when a peripheral part of the body is involved, since blood supply may be poor there.
Time Off from Work After Surgery
There is often a lot of confusion about how a patient should know whether or not to return to work after an injury or surgery. Surprisingly, this decision is generally up to the patient, and NOT the doctor.
Dr. Hyman is authorized to recommend that patients refrain from operating machinery (including driving) while under the influence of anesthesia or substantial mind-altering medication, eg, immediately after surgery or in an emergency situation. Usually we recommend patients avoid driving from the time of surgery until their 1st follow up visit
Doctors determine what IMPAIRMENTS a patient may have and lawyers determine what DISABILITIES a patient may have. Thus, IMPAIRMENTS are defined medically and DISABILITIES are defined legally. There is a big difference between the two.
Usually, we recommend patients avoid driving from the time of surgery until their 1st follow up visit. Dr. Hyman will identify impairments you may have, as a result of your surgery or injuries, and give you restrictions and activity modifications to follow, irrespective of whether you work or not, or what you do on a day to day basis; i.e., if you are told to avoid squatting or climbing or lifting 10 lbs. That applies whether you are a pilot, a schoolteacher, a hockey star or homeless.
Most people are not totally disabled from working, even though they may be impaired by their condition. They may be partially disabled, and only fit for 'light duty' as long as the restrictions are in place, but true disability is really determined in a court of law.
The reason for this is because jobs vary greatly: if you injure your fingers and can’t bend them for a few days, you would be considered by a doctor as having a hand impairment. You would be considered legally partially disabled if you were a typist, because you would be unable to type, but if you were an anchorman on the 10 o'clock news you might not be considered disabled at all, because you could still do your regular job.
The restrictions you'd get from the doctor: no gripping, pushing/pulling/carrying etc, would be the same regarding what's best for your hand, but you and your boss would have to decide if you should work or not. That is technically NOT the doctor's decision.
Doctors don't know all the details of everyone's job, so they give the patients their restrictions and leave it up to the patients and their employers to use their judgment.
Dr. Hyman will assign your restrictions based on your injury, primarily with consideration of the nature of your job, but it’s up to YOU and YOUR EMPLOYER whether or not you can work within the scope of those restrictions. If there is modified work available to you, then YOU decide whether or not you are going to do it. If no such 'light duty' work is available to you, then you or your employer can decide if you should go to work get transported to work, or work at home or whatever. Don't be bullied by threats of losing your job, money or benefits.
Contact your Employer's human resources division if you need further explanation.
Hip Arthroscopy FAQs
After Surgery:
- Can I drive after my surgery?
- How soon can I fly after surgery?
- Can I smoke after surgery?
- When can I go back to work after surgery?
- What is the CPM and why do I need it?
- When do I start Physical Therapy, how often and how long?
- Should I use heat or ice after surgery?
- When can I bear weight, and how long will I have crutches?
- Can I walk up and down stairs at my house?
- If my surgery is later in the day, can I eat in the morning?
- What is the success rate for the surgery?
- Are there certain positions or activities I should avoid?
- What will be the hardest thing to do, i.e. sitting, standing, or lying?
- If I need a bursectomy, how will you know? And what happens without it?
- What is Lovenox therapy?
- How long does the repair last?
Can I drive after my surgery?
Typically, one would have difficulty driving for about 2-3 weeks, though you might be able to drive short distances within a week after surgery. It all depends on pain, swelling, stiffness, type of car, side of surgery: right vs. left, etc. Most patients do NOT drive AT LEAST until after their first postoperative visit (7-10 days after surgery). Even then, caution should be exercised, especially if you are on pain medication or if mobility is limited.
Reflexes and coordination are often somewhat impaired for several weeks after surgery, so care should be taken to drive slowly, with extra distance between cars, etc.
Most people are able to resume relatively 'normal' driving about six weeks after surgery.
You must regain adequate muscle control for braking and accelerating before you try to drive.
Contact your auto insurance company to see if they have any additional restrictions/exclusion clauses on driving after surgery.
How soon can I fly after surgery?
For surgery on the arms and upper extremities, the risk of developing blood clots after surgery is thought to be very low. The true risk is unknown, but in my experience, flying one week after surgery is fine. I've never known anyone to get a blood clot following those guidelines.
Can I smoke after surgery?
Smoking can take a significant toll on the musculoskeletal system. A growing body of research states that tobacco and nicotine increase the risk of bone fractures and interfere with the healing process. Nicotine can slow fracture healing, interfere with estrogen effectiveness and counter the antioxidant properties of vitamins C and E. At a 2002 meeting of the American Academy of Orthopaedic Surgeons, research on the topic of smoking and its effect on the musculoskeletal system was reviewed. Some of the orthopaedic problems caused by smoking include:
- more severe disc degeneration
- weakened spinal ligaments
- reduced production of bone cells
- faster bone loss in post-menopausal women
- fractures take longer to heal
- rotator cuff surgery is less successful
- longer healing time for surgical incisions
- more post-surgery complications
- delayed spinal fusion
Quitting smoking seems to improve the healing process in most cases, except for long-term, heavy smokers who have permanent artery damage, according to researchers. Those with permanent damage due to smoking may not heal easily when a peripheral part of the body is involved, since blood supply to the area may be poor.
When can I go back to work after surgery?
This is another question to which the answer is: “it depends.”
Doctors determine what impairments patients may have, and lawyers determine what disabilities patients may have. Thus, impairments are defined medically and disabilities are defined legally. There is a big difference between the two.
I will assign your restrictions, based on your injury and course of treatment, taking into consideration the nature of your job. It will be up to you and your employer to determine whether or not you can work within the scope of those restrictions. If there is modified work available to you, then you must decide whether or not you are going to do it. If no such "light duty" work is available to you, then you or your employer can decide if you should go to work, work from home or simply take time off. Contact your employer's human resources division for further clarification.
What is the CPM and why do I need it?
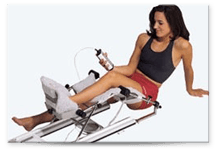
CPM stands for continuous passive motion and it is a machine that will move your hip through a passive range of motion, as opposed to an active range of motion in which the patient does the work. The reason behind using a CPM is to increase blood supply to the affected area, which in turn promotes healing by bringing oxygen and nutrients to the area. You will be given the parameters for the range of motion after surgery but typically will not exceed 90 degrees hip flexion. A DME (durable medical equipment) company will contact you regarding your benefits and if you have an out of pocket expense in regards to the CPM. It is not mandatory you get the CPM however it is beneficial and recommended.
When do I start Physical Therapy, how often and how long?
You can start PT as early as 5 to 7 days after surgery. Depending upon your specific condition, you may start PT before you see Dr. Hyman in the office, but most patients have their first PT visit on the same day they see him back in the office. You will go 2 times a week for the first 6 weeks. The rate will gradually decrease as you heal and become more independent with home exercises. Dr. Hyman has specifically trained physical therapists regarding his hip protocol.
Should I use heat or ice after surgery?
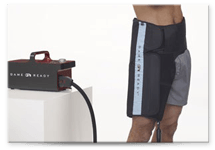
Always use ice! Heat increases blood flow and can cause increased inflammation and swelling. Heat is not indicated until weeks to a month or two after surgery. You will be contacted by a DME company regarding a cryotherapy unit. Cryo=cold. This is a service Dr. Hyman prescribes for his patients. However, not all insurance companies cover this cost therefore it is not mandatory that you get it. If you already have an ice pack at home, that should suffice.
When can I bear weight, and how long will I have crutches?
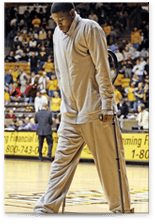
Everyone will be Non-weight bearing (NWB) for the first 1-2 weeks after the surgery. This is because your muscles are in 'shock' and coordination/balance are off. Most patients progress to toe touch weight bearing in week 2-3 and are off crutches completely by 3-4 weeks. However, if osteoplasty (shaving of the bone) is done, you may be NO weight bearing for the first 3-4 weeks. If a labral repair is done, crutches may be needed 4-6 weeks. During this first 4 to 6 week period you will be walking around very slowly and sore. At about 6 weeks, most patients are ambulating normally and you can gradually increase the hip range of motion above 90 degrees. You will receive crutch training at the hospital during your pre-op visit.
Can I walk up and down stairs at my house?
Yes. However you will need to take them slowly and carefully, i.e.: one at a time. Navigating them may be a little tricky, so it is not advised to make multiple trips during the first couple of weeks.
If my surgery is later in the day, can I eat in the morning?
Generally, patients do not eat after midnight the night before their surgery. The reason for this is so there is not food/acid in your stomach for at least 8-10 hours prior to going under anesthesia. If you had food/acid in there, it could cough up into your lungs during surgery and that wouldn't be good. Since there is always a chance that your surgery could be suddenly moved up to earlier in the day, we generally advise patients NOT to eat after midnight regardless of when their surgery is.
What is the success rate for the surgery?
Of course it is patient dependent, but our overall success rate is in the 90-95th percentile range. Generally, the more arthritis and cartilage damage you already have, the less favorable the outcome. For more information on outcomes, see our Research page.
Are there certain positions or activities I should avoid?
Yes, you should avoid flexing your hip greater than 90 degrees (a right angle) for the first 6 weeks. You should also avoid the splits! Intimacy may need to be modified for the first couple of months after your procedure. Avoid having to bend all the way over to tie up shoes (wear slip-ons, sandals, flip flops, etc. – safe but comfortable shoe wear). Avoid very low beds, chairs, car seats and toilet seats if possible. No squats or lunges. Avoid these things for at least 6 weeks after surgery.
What will be the hardest thing to do, i.e. sitting, standing, or lying?
This is patient specific. Some patients find sleeping and lying the most difficult due to not being able to find a comfortable position to sleep at night. Standing may be more difficult for others; as you become more active you may become sore.
If I need a bursectomy, how will you know? And what happens without it?
Typically Dr. Hyman makes the decision to inspect, debride or repair the bursa and associated tissue at the time of surgery based on appearance and your history and pre-op examination. It is removed and eventually 'grows' back. So there are no long-term issues with having it removed.
What is Lovenox therapy?
Lovenox is an injectable drug used to prevent, not treat, DVT or deep vein thrombosis, aka blood clots. Blood clots typically form and settle in the lower leg or calf muscle area as a result of blood not circulated and congealing. This can happen during or after surgery, when your body is trying to clot its blood to minimize bleeding during or after the procedure. It can occur because blood flow is slow when you are not moving around as normal, and Dr. Hyman performs minimally invasive surgery but there is always a risk, albeit low.
Measures are taken so this doesn't happen. Those include pumping your feet up and down as if pumping the gas in a car, taking Aspirin daily, or wearing TED hose (ThromboEmbolicDevices) or SCD (sequential compression devices). We also encourage having the patient up and moving/ambulating as soon after surgery as possible. But if you are at high risk for forming a blood clot, Lovenox will be prescribed. The medication is administered twice a day via a small shot that is given in the subcutaneous area, typically the fat in the stomach.
Click Here to download the Bleeding & Clotting Risk Factors PDF form.
How long does the repair last?
That is a question for which there is no real answer. Long term outcomes, i.e. many years down the road, are not well known. The short-term results seem great and we are seeing more and more success with time. We do however, have evidence to believe that the more damage that is in the hip, especially in the cartilage, when you have arthroscopy, the less likely it is that your hip will last you forever. For more information on outcomes, see our Research page.
For more information on what to expect for your surgery, please see The Surgery page.